foot arch problem
Side Bar
Foot arch problem

FLATFOOT
Flatfoot deformity (also referred to as flat feet, pes planus, pronated foot, and fallen arches) is a deformity that can cause pain and affect people with varying levels of physical impairment. This condition can be in one or both feet and is characterized by no visible arch in the foot when standing. The entire sole of the foot touches or almost touches the ground.All babies have flat feet at birth, with the arches of the foot typically appearing around the age of six. Flatfoot deformity can be genetic or can develop over time. The development of flat feet later in life is called acquired adult flatfoot deformity
Acquired Adult Flatfoot Deformity (AAFD)
An acquired adult flatfoot deformity is a condition resulting from the progressive flattening or collapse of the arch of the foot. It usually occurs as the posterior tibial tendon wears down, or experiences a tear. AAFD can cause pain, swelling, and deformity in the inside of the ankle and the hindfoot, which can become worse without treatment, leading to a complete collapse of the arch.
Stages of AAFD
First Stage - Inflammation and symptoms of an irritated or aggravated posterior tibial tendon. At this point, the tendon is still functioning.Second Stage - This stage shows a change in the alignment of the foot, most noticeably when standing. At this stage, it is relatively easy to restore the foot to its normal position. Most people with acquired adult flatfoot deformity usually seek treatment around this stage.
Third Stage - In the third stage, the flatfoot deformity becomes more significant due to the effect of arthritis. Arthritis develops due to prolonged deformity without treatment, which irritates the joints.
Fourth Stage - the fourth stage, the deformity extends past the foot into the ankle joint, causing swelling, arthritis, and pain. The ankle becomes unstable as the deltoid ligament (the supporting structure on the inside of the ankle) becomes weak, and causes a displacement of the weight-bearing forces.
Types of Flat Feet
Flat feet can cause problems regardless of the age of onset. Both children and adults can struggle due to flatfoot deformity. There are several types of flat feet, which include
● Flexible flat feet: This is the most common type of flat feet, where the arches of the feet are visible when there is no weight being put on them. In other words, the arches only disappear when standing. Flexible flatfoot usually develops during childhood or adolescence and can get worse with age.
● Rigid flat feet: A person with rigid flat feet has no arches in their feet regardless of whether they are standing or sitting. Like flexible flat feet, this condition also develops during the teenage years and gets worse over time. Rigid flat feet can also cause pain and make it difficult to flex the foot.
● Adult-acquired flat feet:strong> As mentioned before, AAFD is a result of the foot’s arch dropping or collapsing. The onset of AAFD can be sudden and can sometimes affect only one foot.
● Vertical talus: strong> It is a congenital disability (birth defect) that prevents the foot arches from forming. It occurs when the talus bone in the ankle is in the wrong position. Since the bottom of the foot resembles a rocking chair, it is often referred to as a rocker-bottom foot.
How Do Flat Feet Affect Your Health?
The feet are not just necessary to maintain an active life, but also for support, balance, posture, and mobility. As such, having flat feet significantly impacts your overall well-being. Having food problems can also affect your knees, hips, lower back, and spine.Flat feet can cause other conditions like plantar fasciitis (overstretched tendons in the feet) and overpronation (ankles rolling inwards). Both these conditions can cause moderate to severe pain, but more importantly, can cause issues with your spinal alignment
The most common ways problems in your feet can affect your body are:
● Back and Joint Pain. If you suffer from any foot problems, you’ve likely adjusted the way you walk to reduce pain. This can cause issues in your back due to misaligned walking problems.
The arch of the foot also helps to absorb the shock of walking, running, jumping, etc. Without the arch, the joints in your body—especially the knees and hips—absorb the shock. Since they aren’t designed to absorb this shock, it can result in severe ankle, knee, and hip malfunction if left untreated.
● Leg Pain. Your feet contain several muscles, tendons, and ligaments that connect to the rest of your body, meaning that pain in the feet can travel into the legs. Stiffness, pain, or weakness in the calf muscle can sometimes be attributed to the foot.
● Posture and Imbalance Problems.strong> Improperly aligned feet can throw off your walking style and patterns, which can cause problems with balance, and make you more susceptible to falls and injury.
Additionally, poor posture is more likely to develop in people with foot problems—the redistribution of weight to avoid the painful parts of the feet can cause poor posture that becomes habitual over time
Causes Flatfoot Deformity?
Flat feet can be genetic or acquired, but some of the most common causes are:- Rheumatoid Arthritis
- Achilles Tendon Injuries
- Cerebral Palsy
- Down Syndrome
- Broken Bones
- High Blood Pressure
- Obesity
- Diabetes
- Pregnancy
- Overuse
- Age
- Lack of Foot Exercise (In Infants and Children)
Symptoms of Flatfoot Deformity
The most identifiable symptom of flat feet is a noticeable lack of arches in the foot, especially when weight-bearing. Pain is also a common symptom, but it may not be present in the early stages. Certain types of flat feet can also be more painful than others.The most noticeable symptoms of flat feet are:
- Inflammation
- Knee, hip, and lower back pain
- Rolled-in ankles.
- Shin splints.
- Bunions
- Hammertoe
- Arthritis.
- Plantar fasciitis.
Treatments for Flat Feet
A flatfoot deformity is a condition that doesn’t go away completely, but many people may not require treatment since they only face mild or no issues. Unless there is a significant level of pain or physical abnormalities, there isn’t much of a reason to be very concerned.However, if you are experiencing pain or other symptoms that get in the way of your daily functioning, contact your healthcare provider to discuss your options. People rarely need surgery to fix flat feet, so your healthcare provider will likely recommend non-surgical methods.
The best treatments for flat feet involve providing support to the arches of the foot and strengthening the foot and ankle. These treatments include:
● Nonsteroidal anti-inflammatory drugs (NSAIDs). Many of these medications are available over-the-counter and can help with pain and inflammation.
● RICE (rest, ice, compression, and elevation).
● Physical therapy can be used to strengthen the feet and ankles. There are also various exercises to help correct flat feet, but make sure to consult your doctor first.
● Supportive devices—custom insoles for children and orthotics for adults can help support the feet. Foot and leg braces can also be helpful. Additionally, the right footwear is essential for people with flat feet. Using the wrong type of footwear can aggravate your issues further.
● Exercise and diet. Getting the appropriate nutrition and physical activity can help improve strength, flexibility, and mobility. For people with obesity, weight loss can help reduce the strain on the foot and ankle by reducing the load.
If non-surgical treatments aren’t relieving or managing your pain, it may be time to consider surgery as an option. Surgery can be used to restore the shape and alignment of the foot and can include the transference of a tendon or cutting and repositioning bones.
When it comes to children, surgery can help prevent any developmental complications in the future.
The recovery period for surgery usually depends on the procedures done, but it typically takes around six weeks to heal. During this time, the patient will be required to keep from putting any weight on the foot. Once the foot has healed, the patient can begin the process of rehabilitation.
HIGH ARCH FOOT
A cavus foot (also called pes cavus) is one that has a very high arch. The problem with having a high-arched foot is that it places too much weight on the ball and heel of the foot. This alteration in your foot’s weight-bearing surface can often lead to pain and instability. Cavus foot is often present at birth, although it can develop at any age. It can affect one or both feet.
Cavus Foot Symptoms
The arch of the foot will appear higher than usual. Not everyone with cavus feet as symptoms, over time, metatarsals (the long bones between your ankle and toes) can start to shift, causing you to become symptomatic. In addition, one or more of the following symptoms may occur:
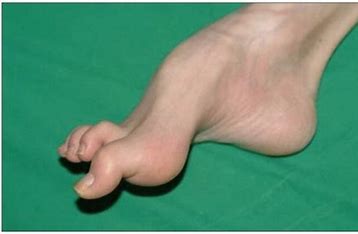
- hammertoes
- Claw toes
- Callus formation on the ball, heel, or along the outer edge of the foot
- Planter Fasciitis
- Foot instability due to an ankle that tends to roll outward
- Foot pain
Causes of Cavus Foot
More often than not, a cavus foot is an inherited structural problem that has no link to any medical condition. However, in some patients, cavus foot can be due to neuromuscular diseases that cause muscle contractures that draw the ball of the foot closer to the heel.
Neurologic conditions causing cavus foot deformity include Charcot-Marie-Tooth disease (CMT accounts for 50% of the neurologic cases), cerebral palsy, clubfoot, post-stroke paralysis, spina bifida, muscular dystrophy, and, rarely, poliomyelitis.
In some cases, cavus is due to a tendon tear of the peroneal tendon which results in cavus deformity.
Although cavus feet, no matter what their origin, can be painful, those due to a neurologic cause tend to get worse faster. As such, they require more monitoring and pro-active treatment in order to prevent progressive foot deformity.
How is Cavus Foot Diagnosed?
Foot and Ankle Surgeon will start by taking a comprehensive medical history and family history to determine if there are any possible neurologic conditions or hereditary factors at play.
Feet will be carefully examined to evaluate their structure as well as to look for calluses or hammer and clawing toe deformities. X-rays may be ordered to look for signs of arch collapse or bone shifting.
Treatment for Cavus Foot
The treatment of pes cavus has a lot to do with the cause and severity of the condition.
Conservative treatment options include:
Modifying your shoe choices
Shoes having thick flexible soles, wide heels no more than 2 inches high, a wide toe box, and shoelaces that can be loosened to accommodate a high arch all help mitigate pain symptoms
Custom orthotics
These are customized insole placed inside your shoe to provide cushioned arch support while correcting your foot position at the same time.
Ankle braces
Braces may be prescribed to provide stability and prevent excessive supination (ankle rolling out).
Physical therapy
PT may be ordered to teach you how to stretch your plantar fascia and Achilles tendons, and also strengthen the muscles and ligaments of your foot and ankle.
Whereas most hereditary cavus feet do fairly well with conservative treatment, in cases where an underlying neurologic condition exists, conservative therapy might fail to provide continued symptom relief as the disease progresses.
Surgery is not uncommon and is an option when other treatments aren’t successful. For surgery for cavus foot, the surgeon will realign the foot to restore function and muscle balance.
