Planter Fasciitis
Side Bar
Planter Fasciitis
plantar fasciitis is the most common cause of chronic heel pain in adults, affecting both young active patients and older more sedentary individuals.It results from chronic overload of the plantar fascia. It can be due to overuse, as seen in runners and military personnel, or due to excessive loading, as seen in obese , sedentary individuals and those who stand for prolonged periods of time. Plantar fasciitis occurs more frequently in individuals with structural foot deformities, including flatfoot, foot with high arch, and leg length discrepancies, each of which are associated with tightness of the intrinsic foot muscles or heel cord. Planter fasciitis more often affects only one foot, although approximately 30% of patients have bilateral symptoms.
Structure and Function
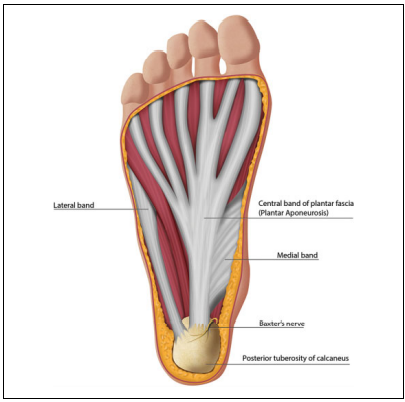
The plantar fascia is a thick band of tissue spanning the arch from the back part of the calcaneus to the bases of the toes. Progressive age related change in this tissue structure leads to planter fasciitis . The plantar fascia originates at the medial side of the calcaneus and inserts at 3 locations in the forefoot, creating 3 distinct bands: medial, central, and lateral (. The medial and lateral band are rarely involved in planter fasciitis. The central band (aka the plantar aponeurosis) is the thickest, strongest, and most often involved in planter fasciitis. It divides into five bundles at the midtarsal level, with each band attaching to proximal phalanges, which in combination with the osseous structures of the arch effectively creates a truss. The plantar fascia is responsible for raising and stabilizing the arch during gait bending of the toes that occurs during terminal gait leads to tightening of the central band of the plantar fascia.
There are a number of foot deformities that predispose individuals to develop planter fasciitis through induction of pathologic biomechanical stresses.
For example, a tight Achilles tendon restricts ankle movement during the late phase of gait, thus blocking forward progression of the center of mass. Patients may compensate for the lack of ankle movement by increasing motion through the subtalar axis , this leads to increased stress in, and eventually attenuation of, the plantar fascia and the other musculotendinous structures supporting the arch leading to the development of planter fasciitis .
In contrast, the high-arched foot has restricted mobility through the foot joints, leading to an inability to dissipate shock from ground strike, thus increasing the load in the plantar fascia, and leading to plantar fascia overload.
Pathophysiology
Previously, PF was thought to occur from a mechanical injury in which excessive tensile strain within the plantar fascia produces microscopic tears leading to chronic inflammation. However, current understanding is that PF occurs through a degenerative rather than an inflammatory process, where tensile strain is the key feature in the pathogenesis.
CAUSES OF PLANTER FASCIITIS
1.Neurologic Peripheral neuropathy (idiopathic, diabetic, nutritional)
- L5/S1 neural foraminal impingement or lumbar spinal stenosis
- Tarsal tunnel syndrome
- Baxter neuroma (neuritis)
2.Traumatic Plantar fascia tear / rupture Calcaneal stress fracture
3.Rheumatologic causes
- Rheumatoid arthritis
- Reactive arthritis
- Psoriatic Arthritis
- Seronegative spondyloarthropathy
4.Degenerative
5.Fat pad atrophy
SYMPTOMS
Typically, patients report a dull aching or throbbing pain, which is localized to the area around the heel.
This pain is usually worst with the first step in the morning and when getting up from sitting. It often gets better with activity, but then worsens as the activity becomes prolonged.
When a patient does not report these classic findings, there should be other causes of heel pain . Heel pain that is described as burning or an electric shock is often neurologic in origin—either from peripheral neuropathy or a compression neuropathy( Disc Prolapse/Disc Budge ) . The compression can occur at a peripheral nerves supplying sensation to the heel.
Compression at the L5/S1 neural foramen is relatively common and may be caused by either degenerative disk disease or facet hypertrophy leading to neural foraminal stenosis.
Compression at the level of the nerve root is often associated with back pain, radicular leg pain, or sensory loss in the foot or leg.
Tarsal tunnel syndrome typically presents with burning or shocking pain along the plantar aspect of the foot and is often associated with numbness along the plantar surface.
Baxter neuropathy is a compressive neuropathy of the first branch of the lateral plantar nerve characterized by burning across the heel pad.
The presence of a suspected compressive neuropathy may be confirmed by imaging and/or electromyography, but should be initially evaluated with a focused physical examination.
In the case of Baxter neuritis, the diagnosis is confirmed by magnetic resonance imaging (MRI).
Traumatic causes of plantar heel pain include plantar fascia tear or rupture and calcaneus stress fracture. The pain of a plantar fascia tear is often located within the midportion of the plantar fascia.
The presence of a calcaneus stress fracture should be suspected in a patient who has a history of osteopenia, other stress fractures, or fragility fractures.
The presence of bilateral heel pain, heel pain concurrent with multiple painful or stiff joints, or a stiff spine suggest a rheumatologic etiology.
The seronegative spondyloarthropathies occur most commonly in young.
IMAGING AND LABORATORY EVALUATION
Weight-bearing radiographs of the foot are often obtained at presentation to evaluate foot alignment, exclude bony lesions, and determine the presence of a plantar heel spur
The heel spur is a sign of calcification at heelpad. It is seen in a number of disorders but is of no functional significance, as neither the shape of the spur nor its size correlates with symptoms of planter fasciitis.
It has been suggested that radiographs are not needed in the initial evaluation of heel pain as the vast majority are either normal or show only a heel spur.
Soft tissue imaging is not routinely required in the diagnosis of planter fasciitis.
The goals of soft tissue imaging are to confirm the diagnosis of planter fasciitis and to exclude other causes of heel pain such as inflammatory arthropathy (spondyloarthropathy), Baxter neuritis, and calcaneus stress fracture.
Ultrasound provides a rapid and cost effective means to confirm the diagnosis of Chronic planter fasciitis.
A plantar fascia thickness >4.5 mm and the presence of hypoechoic areas are specific for Planter fasciitis.
The extent of reduction of fascia thickness is an objective measure of treatment efficacy, as thicker plantar fascia correlates with increased symptoms and patient-reported pain scores on VAS.
MRI can be also be used to confirm the presence of PF with characteristic findings of increased signal intensity and proximal plantar fascia thickening
MRI is most useful in excluding the presence of other causes of heel pain such as calcaneus stress fracture, Baxter neuritis, tarsal tunnel syndrome, and insertional Achilles tendinopathy.
Electromyography (EMG) can be used to evaluate suspected neurologic causes of heel pain in patients presenting with sensory disturbances.
Chronic neurologic heel pain secondary to local nerve entrapment commonly occurs with the first branch of the lateral plantar nerve and medial calcaneal nerve branches. In these cases, EMG helps to localize the site of entrapment.
LABORATORY EVALUATION
This should include a complete blood count , Kidney and Liver function tests, ESR, CRP( C Reactive Protein), RA (Rheumatoid factor) , ACCP.
MANAGEMENT
Nonoperative Treatment
Planter fasciitis is usually a self-limiting condition, with more than 90% of patients achieving symptomatic relief with 3-6 months of conservative treatment.
Initial treatment should consist of
1.Nonsteroidal anti-inflammatories (NSAIDs)
2.stretching of the gastrocnemius and the plantar fascia
3.Use of an orthosis (heel pads, heel cups, arch supports, or night splints).
Orthotics, heel wedges, and heel cups
Orthotics decrease heel rise and Achilles tendon force during gait, leading to pain reduction. Both prefabricated and custom fitted orthotics have been shown to reduce pain and improve function in the short term with few risks or side effects.
Prefabricated foot orthotics such as gel heel cups, longitudinal arch supports, and full-length shoe insoles have been shown to be more effective than custom shoe inserts.
Immobilization
Night splints and CAM walker boots.
The night splint is an orthosis that prevents plantar fascia contracture by maintaining a neutral position of the ankle during sleep.
Night splinting is most effective in patients whose chief complaint is morning pain.
Ice Fomentation
Ice fomentation with either ice cube or ice packs will help to reduce planter fascia spasm and it should be done with the physiotherapy and at early morning before doing any routine household work.
Physiotherapy
A physical therapist can assist with the treatment of planter fasciitis in a number of ways including reducing pain, guiding stretching exercises, supervising strengthening exercises.
In addition to stretching, the therapist can use manual therapy, consisting of joint and soft tissue mobilization, to improve lower extremity flexibility, to decrease pain, and improve function.
Stretching of the gastrocnemius muscle is a mainstay of treatment of planter fasciitis. This stretching can be either self-directed or guided by a physical therapist
. Moreover, the stretching can be performed either seated or standing, but it must be done with the knee extended.
In the gastrocnemius stretch, the hands are placed against the wall, the leg being stretched is slid posteriorly with the knee bent as far as it will go and then the knee is straightened
In the plantar fascia stretch, the foot to be stretched is placed on top of the contralateral knee, the ankle is maximally dorsiflexed, and then the toes are pulled up, tensioning the plantar fascia.
MINIMALLY INVASIVE TREATMENT
Patients with heel pain for 6 months or more that is to the nonoperative treatments may undergo minimally invasive procedures that relieve pain.
Corticosteroid injection
Corticosteroid injections are often used to treat the pain associated with planter fasciiatis, however, their use is controversial. A number of studies have demonstrated short-term pain relief with CSI; whereas others have found poor results in comparison to PRP injection.
Should you take steroid injection or not?
The rationale underlying the use of corticosteroid injection in the treatment of planter fasciitis has come into question because of the improved understanding of planter fasciitis as a degenerative rather than an inflammatory process.
The therapeutic benefit of corticosteroids is dependent on their anti-inflammatory properties, which provide significant pain reduction; however, they also act to inhibit fibroblast proliferation and ground substance protein expression. These effects can produce atrophy of the plantar fascia and plantar fat pad and can lead to complete plantar fascia rupture, both of which are difficult to treat.
A number of studies have demonstrated the association between steroid injections and plantar fascia rupture.
In summary, steroid injections may provide temporary symptomatic relief but are associated with an increased risk of developing persistent pain, local tissue atrophy, or plantar fascia rupture. Thus, if they are used it should be with caution and patients should be advised of the risks and benefits prior to injection.
Botulinum toxin
Botulinum toxin A
Injections of BTX into the plantar fascia and gastrocnemius-soleus muscles reduce tension in the plantar fascia and may have an analgesic effect and produce muscle relaxation without the risk of rupture that occurs with heel cord–lengthening procedures.
BTX into the gastrocnemius combined with plantar fascia stretching exercises has been shown to produce greater pain relief and functional improvement compared with Corticosteroid injections.
Platelet-rich plasma
PRP has grown in popularity for treating a number of orthopedic conditions, including Chronic Planter fasciitis.
PRP is extracted from autologous whole blood and contains a high concentration of endogenous growth factors.
These growth factors are thought to activate intrinsic cellular mechanisms that restore the plantar fascia.

Shock-wave therapy and intense therapeutic ultrasound.
ECSWT(Extra Corporeal Shock Wave Therapy) delivers low-frequency high-energy acoustic waves to the plantar fascia, which induces microtrauma that activates interstitial and extracellular responses leading to tissue regeneration, angiogenesis, increased blood flow, and nutrient delivery.
Systematic reviews have concluded satisfactory short-term pain relief and functional outcomes, including decreased morning and activity pain, and pain associated with walking.
In contrast, intense therapeutic ultrasound uses highfrequency high-energy ultrasound to create small thermal injury zones inside soft tissue without damage to surrounding structures.
OPERATIVE TREATMENT
Operative treatment is indicated when pain and functional limitations persist despite an adequate nonoperative trial lasting at least 6 months.
Partial Plantar Fasciotomy
Partial plantar fasciotomy is the traditional procedure used in the treatment of Planter fasciitis. It involves partial transection of the planter fascia to stimulate a healing response.
This procedure can be performed either through an open or endoscopic approach. It can be combined with Baxter nerve decompression for medial heel pain where compression of Baxter nerve is suspected.
Minimally invasive partial plantar fasciotomy can be performed using either ultrasound-guided percutaneous or endoscopic techniques.

Gastrocnemius Lengthening
Operative release of the gastrocnemius could result in improved heel pain. Proximal release of the medial head of the gastrocnemius is an alternative technique for lengthening the gastrocnemius. It has been shown to be as effective as gastrocnemius recession and with fewer complications
